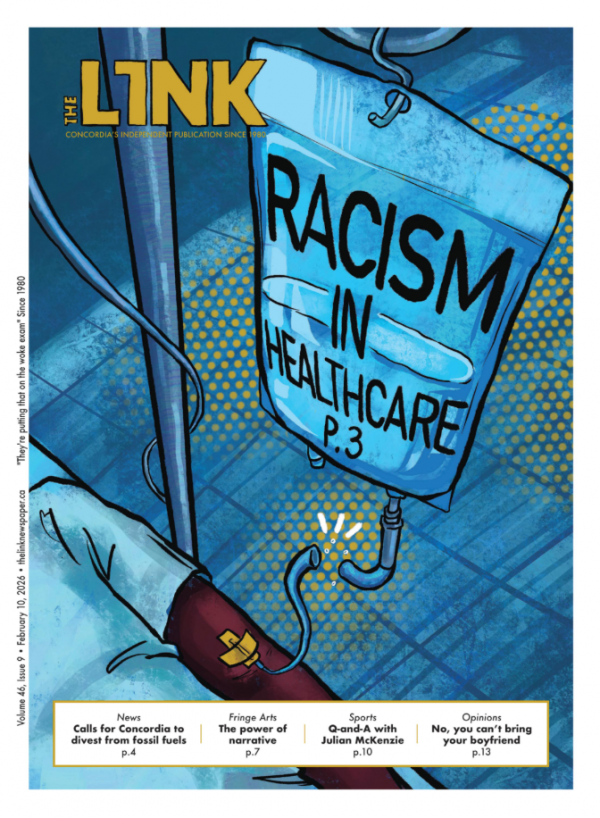
The BIPOC perspective of healthcare in Quebec
Five years after Legault claimed systemic racism does not exist in Quebec, resident testimonies illustrate its existence
Of the many negative healthcare experiences they have had, Montreal resident Peach, who has been granted a pseudonym for safety reasons, recalls a particularly distressing encounter at a medical clinic in the city.
“I walk out, and I'm really shaken up about it,” they recounted. “This whole waiting room of people is looking at me, and I'm standing [there]. I go to the elevator, I'm about to leave, and I'm about to cry.”
After being left with little to no healthcare options in 2020 following their graduation from Concordia University, Peach said they entered Quebec’s Primary Care Access Point (GAP) program, hoping to speak with a healthcare professional about ongoing health issues they were experiencing.
The GAP program led them to the doctor responsible for their jarring experience.
Peach was given just five minutes to explain to the doctor the details of their lower back pain and a cyst they had discovered on their hand. They requested a prescription for a cortisone shot, as they had previously received them every three months to manage their pain.
In response, Peach said this doctor—an older, white man—warned them that getting more than three of these shots a year could lead to diabetes.
“I feel he was only mentioning it because of my weight,” Peach said, adding that prior healthcare professionals had assured them they were “not even close” to being diabetic or pre-diabetic.
Then, when they followed up about the cyst, Peach said they received another upsetting response.
“He looks at it, and then he says, ‘This isn't a medical course, I can't tell you everything that's wrong with you. If you have Google, why don't you go home and just Google it?’” Peach said. “This is so messed up. You cannot tell people to Google their symptoms, that's crazy.”
As a member of the Black, Indigenous, and People of Colour (BIPOC) community, Peach is not alone in experiences such as this.
Angel Uwurukundo is a Montrealer who writes about her experiences navigating systems in the city as a queer Black person with chronic illness on her Substack, Letters From an Angel. Uwurukundo described similar experiences accessing healthcare.
“Honestly, I feel like most of my experiences were like that,” Uwurukundo said. “You go to an appointment, and it’s as though the doctors are very detached.”
Uwurukundo described how she has gone into healthcare appointments with a detailed account of the issues she’s experiencing, even sometimes written down as notes, only to leave the appointment with just one issue partially addressed.
“I have a thousand things going on inside my mind. I have this tightness in my body, and I have an inability to just be in this room with this person, but I have to rely on this person to provide me care,” Uwurukundo said. “I don’t feel as though I was able to advocate for myself in those moments.”
BIPOC healthcare underresearched in Canada
In stark contrast to these firsthand testimonies, in 2020, Quebec Premier François Legault confidently declared that “there's no systemic discrimination” in Quebec.
This statement came just a year after a report commissioned by the City of Montreal concluded that Black and Indigenous people were four to five times more likely to be stopped by police.
Several studies conducted on racial discrimination in healthcare services revealed that Black communities in Canada face significant health disparities, including higher rates of hypertension, diabetes, breast, cervical and prostate cancers, as well as coercive care for psychosis.
A 2022 study on cancer disparities found that, in the domain of cancer research, significantly fewer studies have been conducted to collect BIPOC data: out of the 20 most common cancers in Canada, 15 have no data on Black people.
According to Dr. Akwatu Khenti, associate professor at the University of Toronto School of Public Health, BIPOC individuals face two main hurdles when it comes to receiving healthcare.
The first, he said, is a mistrust of the healthcare system based on lived experience.
“Many surveys consistently report Black patients or Black clients who say that they have experience not being listened to, or they feel disrespected in interactions with caregivers,” Khenti said. “Trust is a barrier to being open and honest about issues, and it’s also a barrier to recovery.”
The second barrier, he added, is implicit bias, stereotypes and stigma, which influence interactions between racialized and non-racialized individuals.
“[BIPOC] students report a lot of experiences with micro-aggressions in medical schools,” Khenti said.
“My problems don’t stop at a better system that is more efficient. My problems stop when Black people, all Black people, are treated and considered like human beings and individuals.” — Angel Uwurukundo, Montreal resident
The nuance of BIPOC medical experiences
Uwurukundo said she often hears from others that she shouldn’t complain because "everyone in Quebec feels the weight of how bad the medical system is.” But for her, the intersectionality of healthcare struggles often goes overlooked.
“That’s something that frustrates me, because I do not even claim that others have it better than me or have more answers to their problems than I do,” she said. “It’s rather that there is a specific experience, as a Black person.”
As a Black person, Uwurukundo said her experiences make her feel alienated from the medical system.
“[Western Medicine] has never been something for us. It’s been tested on us. We have been neglected,” she said.
Uwurukundo said that, in her experience, one of the biggest struggles to improve healthcare for BIPOC stems from the fact that the term "Black" can be too vague.
“Just in Montreal, the Black population is from so many different places,” Uwurukundo said. “To generalize all those Black people when it comes to their health is overlooking a lot of problems.”
Hence, when it comes to general complaints about the Quebec healthcare system, Uwurukundo expressed that she finds she cannot relate to these comments in the same way.
“My problems don’t stop at a better system that is more efficient,” Uwurukundo said. “My problems stop when Black people, all Black people, are treated and considered like human beings and individuals.”
Towards an equitable healthcare system
Khenti said that simply increasing the collection of race-based data can help solve the issue of race-based discrimination in Canada.
“We've seen, during COVID-19, that such data saves lives,” Khenti said. “This [lack of data] is an example of systemic or implicit bias, because the fact that it saves lives doesn’t give it enough legitimacy to [be] instituted by our decision-makers.”
Khenti added that, when it comes to the medical world, an important distinction must be made on "race" not as a biological concept, but as a social reality.
“It’s a social construction that has health outcomes; without that data, we don’t know who has more vulnerabilities than whom,” Khenti said. “The data really allows us to do targeted care, targeted interventions, and save lives.”

._MG_7183_900_677_90.jpg)

_600_375_s_c1.png)


