Navigating intimacy and sex after cancer
Approaching sex post-diagnosis can be intimidating, but far from impossible
Sexology and cancer are sensitive topics, but how they intersect is discussed even less.
The treatments against cancer can be very aggressive and often leave damaging repercussions on one’s body. They affect all aspects of people’s everyday lives, notably their attitudes towards sexual health and intimacy.
An introduction to oncosexology
In Quebec, there are very few people specialized in oncosexology, a term which refers to sex therapy for cancer patients. Renée Pichette was the first professional to occupy the position of clinical sexologist in oncology in Quebec.
“It’s Dr. Pierre Drouin that approached me to do a small survey since he felt that oncology disorders had repercussions on women’s sexuality,” said Pichette about the beginning of her career as a clinical sexologist.
At 39 years old, and after working as a medical secretary, Pichette decided to go back to university to obtain a bachelor’s degree in sexology at Université du Québec à Montréal, as well as a clinical master’s degree. She had her first encounter with cancer patients during her internship at the Notre-Dame Hospital in Montreal. There, she worked with women experiencing problems mainly linked to vulvar vestibulitis and needed colposcopies—a procedure used to examine the cervix, vagina, and vulva for signs of diseases, like cancer.
After being approached by Dr. Drouin, who specialized in gynecologic oncology at the Centre hospitalier de l'Université de Montréal, Pichette got involved in a project regarding the creation of a psychosexual clinic in oncology around 2001. She explained that due to the hard work and tenacity of the gynecologic oncology team, the project continued to evolve, which eventually led to the creation of her position as a clinical sexologist in oncology at the CHUM in January 2008.
“In the [Quebec] healthcare system, in oncology, we are three, maybe four. We are not a lot,” said Pichette, on the number of clinical sexologists practising oncology in the province.
The few clinical sexologists working in oncology departments like Pichette follow their patients throughout the entire time they are being treated against cancer, which can go anywhere from months to years.
“The goal is really to bring the person through a process of psychotherapy, through reflections, [and] through a journey in which we accompany the person,” she said. “In oncology, we are also subjected to medical monitoring. […] We follow the evolution of the patient.”
Outside of hospitals, it is still possible for people going through treatments or in remission to receive counselling from psychotherapists in sexology.
It is also possible to receive counselling from interns like Marianne Laporte, a third-year student in the department of sexology at UQAM. Amidst the framework of her internship, she became interested in the medical and biological aspects of sexology, and the relationship of these aspects among people struggling with cancer treatments.
Laporte does individual and couples counselling, as well as group counselling for women. She explained that her goal is to help people gain back their ability to feel confident in their sexuality after it has been affected and altered by cancer treatments.
“I have clients that don’t know if they will survive. They still have cancer and it’s not necessarily a good diagnosis since they may pass away eventually,” she said. “But they still seek help so that these moments—[whether they] be one to two years or 10 to 20 years—[are spent] the way they actually want.”
“Every time my partner would touch my breasts, I would remember how I’d had an operation, [the reason] why I had the operation, [and my] cancer remission.” — Julie
Repercussions of cancer treatments
Receiving a cancer diagnosis is a very traumatic and difficult moment to go through. In some cases, decisions have to be made quickly regarding treatments and surgeries. Good sexual health isn’t something that comes up when receiving a diagnosis. It often comes later in the process after the treatments have already affected the body.
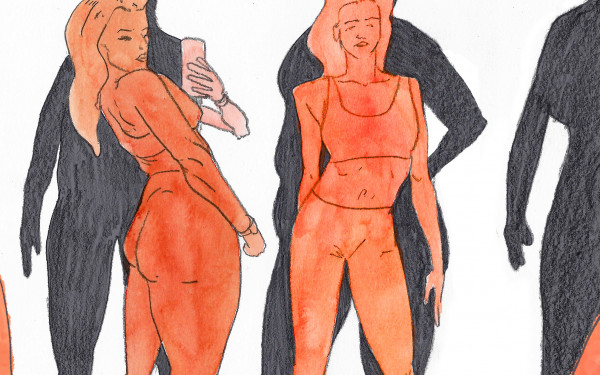
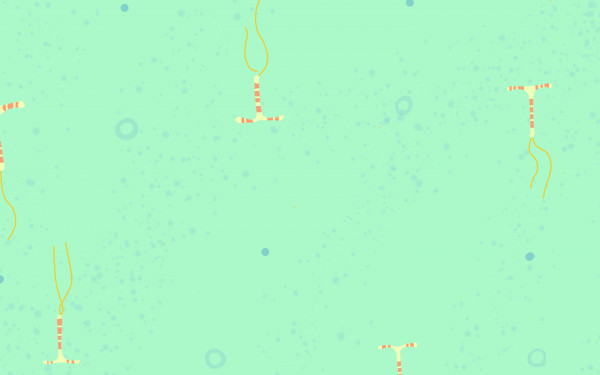
The repercussions of cancer treatments often lead to sexual dysfunctions for patients. Among other treatments and surgeries, hormone therapy is a treatment used to slow or stop the development of cancers that need hormones to grow, which are found in breast or prostate cancers. The side effects of this treatment can cause the decrease or loss of sexual desire, the inability to have an erection, as well as menopause-like symptoms including vaginal dryness, hot flashes, and changes in menstruations. These reactions can alter the sexual health and capability of patients, which can lead to psychological distress and changes in a couples dynamic and intimate habits.
“[In my relationship], the breasts were part of the foreplay, they were kind of a key element,” said Julie, a breast cancer survivor, who agreed to share her story anonymously and whose name has been changed for the purpose of this article. “Slowly, what happened was that every time my partner would touch my breasts, I would remember how I’d had an operation, [the reason] why I had the operation, [and my] cancer remission, and right away there were all these thoughts going through my head.”
Julie was diagnosed in her early 30s, not long after having her first child. She explained how consulting a sexologist helped her find solutions for the physical aspects of her sexual dysfunctions, but also helped her deal with the trauma and anxiety that affected her intimacy.
“[I was] feeling aged in [my] sexuality, and in my head I wasn’t accepting it,” Julie said. "I still felt young, and my partner and I had recently had a child. I wanted to live the way other couples my age were living," she added.
“I wanted to live the way other couples my age were living.” — Julie
A social issue
Pichette explained how cancer has become a chronic problem in our society that demands an important need for qualified sexologists in oncology programs. The need for trained sexologists is crucial since they are able to adequately guide patients in decreasing the psychological distresses linked to a lack of fulfillment in their sex lives.
“The precision of sexologists isn’t for nothing. We are there to help these people adapt better to their situations and to [help them] understand what is happening [in their bodies],” said Pichette. “I hope that one day, every oncology program will have a sexologist on their team, [and] that there will be a trained person who understands sexuality and all its aspects, who will able to help these people regain a balance even if it’s not like before, a balance in the quality of their sex life.”
Pichette remains as passionate about her position in the field as she was 14 years ago when she first started. She explained how there is an important need for funding in order to integrate more sexologists in oncology departments across the province.
“Sexuality is always there,” she said. “It is innate [and] fundamental to humans, and we have to take that into consideration in the context of oncology.”
This article originally appeared in The Body Issue, published February 1, 2022.