We Are Failing to Deal With the Opioid Epidemic
Lack of Discussion Around Mental Illness Has Worsened the Drug Crisis
We can no longer deny the severity of the opioid crisis.
As the epidemic continues to take the lives of opioid-related users, we need to recognize how we are addressing it and how we can combat overdoses more actively.
Our governments, education systems, and society as a whole are failing by not providing an adequate teaching and understanding of mental health, addiction, and how the two intertwine.
It wasn’t until months after a friend had passed that I came to realize that lack of education in our institutions and society had not only failed so many, but that it had directly failed him in particular with his struggles with mental health and addiction.
Like many people in our society, he had unfortunately leaned on certain substances to temporarily increase his happiness and ease internal struggles. However, it only led to addiction and furthered battles with mental illness.
Last summer when I attended his funeral, I became overwhelmed with the fact that this situation isn’t one of a kind; it can easily happen to so many people. Regardless of the abused substance, the fact that our society and institutions provide limited knowledge on the connection between addiction and mental health, as well as how to identify mental health issues at a young age is extremely problematic.
As the National Institute on Drug Awareness details, addiction is a mental illness which changes the brain in fundamental ways, as the regular needs of a person are distorted to fit the needs of the drug. These uncontrollable behaviours which override the control of impulses, despite consequences, are related to characteristics of mental illness.
Dr. Warren Steiner, a practicing psychiatrist who works at Montreal rehabilitation centre Homewood 360dtx said it is very complex to say that addiction is initiated by mental illness, because they are both very intertwined.
However, Steiner explained the connection can be identified in the way neurochemistry of substance use is very similar to the neurochemistry of mental health problems.
“We’re dealing with a small number of brain chemicals—adrenaline, dopamine and serotonin—and those are the ones that go off balance in many mental illnesses and those are the ones that drugs of abuse play with.”
Just as depression and anxiety are imbalances of serotonin levels, Steiner identified that drugs like MDMA spike and temporarily deplete natural serotonin levels. A result of addiction to a substance like MDMA, when a user is in withdrawal, the overuse of serotonin levels can mimic depression.
Steiner said psychiatrists used to refuse treating patients with addictions until they became sober.
“We understand now that these disorders are very, very intertwined and you can’t just treat the mental illness and you can’t just treat the substance abuse,” said Steiner.
For a successful outcome there needs to be a program and medical approach that will address both at the same time, he said.
In my freshman year of highschool, I began to recognize the changes some of my friends were going through. When some were left undiagnosed or not given the proper attention and treatment, I saw them turn to drugs.
As powerless as I felt in my attempts to support and resolve their issues with mental illness and addictions, I witnessed the years of struggle with therapists, doctors and sometimes rehabilitation centres. And even the personal struggle of those who did not seek professional support. This demonstrated that recovery is not linear, but it can be a messy situation with ups and downs.
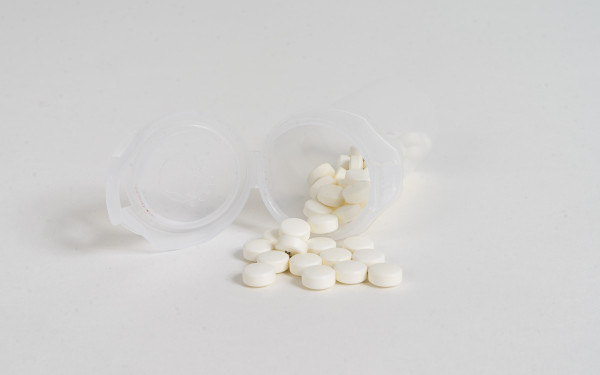
When I began to learn about the opioid crisis, I learned the horrifying truth that many opioid addictions were generated by doctors over-prescribing opiates. The impending opioid crisis grew with an increase of Oxycontin prescriptions—which became abused and often resold on the streets.
When Oxycontin was removed from the pharmaceutical markets in 2012, the singificantly more potent Carfentanil and Fentanyl came to replace Oxycontin. This has lead to a surge in overdoses and opioid-related deaths in the country.
Within the Government of Canada’s publications on national statistics and the government’s plan of action, I found the mention of mental health quite limited or non-existent in most opioid-related documents.
In one document considering the comparison of death rates from 2016 to 2017, it mentioned that the Government of Canada had planned to provide $5 billion over a 10 year period to improve mental health and addiction services.
The document stated the Canadian Institutes of Health Research would be generating a report to provide greater education of issues impacting the opioid crisis, with involvement of mental health experts. However, many other documents considering the opioid crisis failed to connect these issues.
Despite this, I believe that we have been failing to properly address the growing opioid-related death rates for years.
With years of institutions, politicians, and reporters not discussing the connection between drug use and those who fight mental illness, we don’t have a comprehensive understanding of this impending epidemic.
“The problem with politicians is that they often say all the right things, but there’s no action behind that,” said Steiner, referencing U.S. President Donald Trump’s actions towards the opioid crisis.
In October 2017, Trump declared the opioid crisis to be an emergency in America and they were going to do big things, such as introducing “really tough, really big, really great advertising,” Trump said. However, the president did not apply for any funding, according to The New York Times.
“Canada is a little bit better, but politicians move very slowly and they don’t see a lot of votes in addressing substance abuse, so it becomes less of a priority,” Steiner said. “There hasn’t been a lot of money put into school education programs and that’s where you have to do it.”
NDP leader Jagmeet Singh is pushing for Prime Minister Justin Trudeau to decriminalize all drugs in order to properly deal with high rates of opioid-related deaths.
The Toronto Star reported that Singh said opioid-related use is not a criminal issue, however a social justice issue, as Canadians dealing with opioid use are influenced by mental health problems, addiction and poverty.
During a town hall in Edmonton, Trudeau said legalizing all drugs would not be a part of addressing opioid-related deaths, but reminded the crowd marijuana would be legalized later this year.
According to 2013 statistics from the Mental Health Commission of Canada, 3.2 million Canadians between the age of 12 to 19-years-old are at risk of developing depression. Once depression is recognized, treatment can provide positive changes for 80 per cent of people impacted.
The victims are not to blame. The failure within our education system to properly discuss these issues have led to some falling into addictions where they cannot recognize mental illness.
If students cannot recognize mental illness, our lack of conversation and education will lead to a lack of diagnoses. If some find comfort in drugs, it may generate more addictions.
The national death toll for opioid overdoses in Canada accounted for 2,861 lives in 2016. While there have not been national death rates for opioid-related overdoses recorded before 2016, between 2014 and 2015 there were 4,779 Canadians hospitalized or taken to the emergency room for opiate overdoses. This is a 30 per cent increase since the 2007-2008 rates.
While no national data has been released for the total rates for opioid-related deaths in 2017, in December, the Public Health Agency of Canada released a statement detailing that they expect to see the number of opioid-related deaths in 2017 to exceed the number of deaths in 2016.
“Tragically, if current trends continue, we may see more than 4,000 deaths in 2017,” the statement made in December detailed.
While my teachers were attempting to force equations and equilibriums into my brain, the institution failed to provide proper education of a situation that would not only touch my life, but affect thousands of families across the country.
In conversations with others over the months, I found that I wasn’t the only one who had a lack of education on mental health and addiction.
“I don’t remember there being talk of withdrawal or addiction and mental health,” said Raven Francis-Browning, a 21-year-old student in Toronto.
There wasn’t enough advice or scenarios provided to help us recognize addiction and mental health issues within ourselves, Francis-Browning said, adding that if she was educated more then maybe mental illness and addiction would have not impacted her life as much.
Coni Alvarez Fritsch, a 20-year-old student in Toronto said her education on drugs was often limited to the scientific impacts and legal consequences.
While mental health was not addressed within her high school curriculum, it was discussed a bit in announcements, clubs, and mental health awareness week. However, Alvarez Fritsch said there was definitely no talk of it combined with drug use awareness.
“I vaguely remember some assemblies about drug awareness with guests coming to speak about the subject and about mental health, but never at the same time,” said Sean Andrade, a 22-year-old student. “Honestly, I think I learned more about drugs from my friends at school than from anywhere else.”
These are similar scenarios I found myself in. I was slowly failing in trying to help those around me based on the little understanding I had of the situations they were going through, but maybe if I had more education I could have recognized these behaviours and understood how to properly help.
“We know that people with mental health problems are at a higher risk to develop substance abuse problems also, especially if untreated,” said Steiner.
But how are people supposed to understand if they have a mental health problem if they are not taught from a young age how to recognize it? How can they understand if they have an addiction, if they are not properly being educated on it?
I realized that some people around me who have struggled with mental illness who depended on drugs are often reluctant to seek help, sometimes in fear of truly understanding the illness hiding beneath their substance abuse.
“For addiction there is also stigma, because we tend to blame the addict,” said Steiner. As a result, he said this has led and will lead people to hide the truth from their doctors, parents, counselors or teachers.
Steiner said that people don’t want to discuss and recognize mental illness, because as a society we often blame the person with the illness, rather than seeing it like any other illness.
The victims are not to blame. The failure within our education system to properly discuss these issues have led to some falling into addictions where they cannot recognize mental illness.
Regardless of the close relationships I had with some of my friends, I often found they would hide the addictions they were experiencing. Even my closest confidant had trouble admitting to me some of the addictions they battled over the years—possibly as a result of thinking I may shame them or be disappointed.
These are underlying results of the stigma our society has generated, which delays those with mental illness and addiction from seeking help and receiving support from their loved ones.
“The longer that we delay treatment the worse the outcome and the more complex it becomes,” Steiner said. “The conversation isn’t just about mental health anymore, it has to be about both, because you’re going to get improved outcomes.”
With insufficient education, we will only fuel the fire of the opioid crisis.
If the education of mental health and addiction had been more prevalent, I believe some of my friends would have felt more comfortable discussing their battles and seeking help.
If so, maybe my friend would still be alive today.