Montrealers are facing barriers when accessing mental health services
Individuals and communities face different challenges depending on their situation
Quebec Premier Francois Legault has refused to call the mental health situation in Quebec a crisis despite wait lists for public counselling services now exceeding 20,000 people.
This situation is reflective of broader barriers to accessing mental health services across the province. For Montrealers, such barriers manifest in different ways for individuals and communities depending on their circumstances.
Many students at Concordia have complained about barriers to accessing the university’s mental health infrastructure, including long wait times and poor communication.
Concordia’s Counselling and Psychological Services provides individual counselling sessions on a first-come, first-serve basis. Though this process was initially handled in person, appointments now have to be booked online on account of the pandemic.
One Concordia student who wished to remain anonymous said they struggled to book an appointment despite trying for several weeks. “I couldn’t get a spot even if I emailed right at the start of their booking period. I never ended up getting any help,” they said.
“I couldn’t get a spot even if I emailed right at the start of their booking period. I never ended up getting any help,” they said. — Anonymous
According to Gaya Arasaratnam, Director of Campus Wellness and Support Services at Concordia, the university employs only 12 counsellors to accommodate all 52,000 of its students.
“It is important to note that counsellors work with their clients to create tailored plans that meet their needs and goals,” Arasaratnam added in an email. “The frequency and time between appointments is dependent on the students’ needs, and how best counselling can support those needs within our mandate as a short-term counselling clinic.”
Michaela Marjerrison, a third year psychology student at Concordia, attempted to access counselling services provided by the university’s Sexual Assault Resource Centre in February. While she was able to book an appointment, she said the only available slots were a month away, and that her designated counsellor could only offer sessions once every 3-4 weeks.
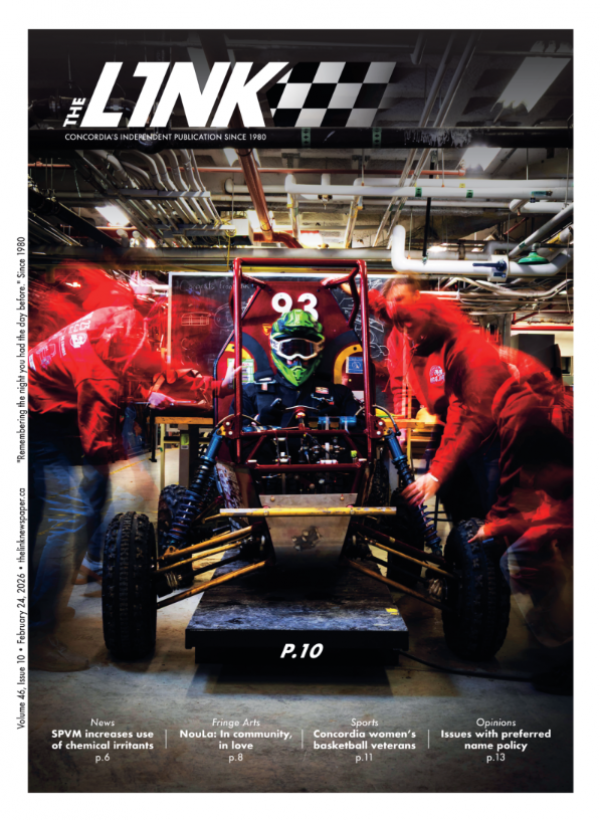
Marjerrison said she then turned to Empower ME, a third party 24/7 mental health hotline available to students as part of Concordia Student Union’s insurance plan.
“I was pretty much completely suicidal at that point and I was like I need a counsellor immediately,” she said. “They said ‘yeah we can get you a counsellor by the weekend’. The weekend came around and I had no phone calls, or emails, or anything and they had my contact info. Absolutely nothing. So I ended up having to go to a mental hospital in Montreal.”
Mary-Elizabeth Kroitor is a third year anthropology student at Concordia who has also attempted to access mental health resources at the university. Kroitor says that she’s grateful to have access to a psychiatrist through Concordia, but that the university’s services are ultimately lacking. “There’s a limited amount of resources which are too few and inaccessible for the people who need them to properly benefit,” she said.
“I think that Concordia’s mental health resources would be greatly improved by a more robust and comprehensive drop-in system, especially if it was translated to an online format,” she added. “It’s important to simplify access to care wherever possible. It’s difficult to navigate bureaucracy and/or extra steps when you’re upset and in crisis.”
“It’s important to simplify access to care wherever possible. It’s difficult to navigate bureaucracy and/or extra steps when you’re upset and in crisis.” — Mary-Elizabeth Kroitor
Arasaratnam explained that Concordia may be open to such a possibility. “I’d be happy to take it under careful consideration and explore what might be possible, even if it’s not exactly a 24/7 drop in clinic, but something that might meet the same goal that students are voicing for higher levels of access,” she said.
However, for members of Montreal’s Black Community, barriers to accessing mental health resources are often more entrenched and harder to overcome.
Kristen Young is an internal coordinator at Black Mental Health Connections (BMHC), an organization that promotes mental health resources for Montreal’s Black Community. She says that many Black Montrealers are hesitant to access the city’s healthcare services because practitioners are often not trained to accommodate their specific physical and cultural needs.
“That's really hard to do in situations where there's already a discrepancy in power between those who are providing services and those who need services,” she added. “I'm not going to enter a situation where I need to tell someone that I'm not doing well in my brain if I don't even know if they would acknowledge when I'm physically not doing well.”
According to BMHC, the best route around these barriers is through community-based support groups where Black Montrealers facing mental health challenges can be vulnerable with each other.
“[The participants] are able to validate in a way that doesn't feed back into power dynamics which for us harkens back to the oppressive systems that we live and can't get away from,” she added. “It’s easier in a group setting to think of it as a community, and that community feeling is something that is really big for us and can be really healing.”
Young mentioned BMHC’s Online Peer Support Group, a mental health program targeting Black LGBTQ+ youth launched last year. She said the program’s emphasis on validating shared experiences and building skills to deal with mental health challenges showed promising results.
“I think it’s a better option for everyone. Specifically for Black people, yes, because community is a large part of our culture,” she added. “But we do have the hope that this will be a framework that is transferable.”
Ella Amir, Executive Director of the mental health clinic Action on Mental Illness (AMI) Quebec, told of a similar approach AMI has adopted for its free online Kaleidoscope support group. She said that the program targets individuals facing a variety of mental health challenges from across Montreal and is successful largely because it’s so easy to access.
“I think that group counselling really has a power that no individual counselling may have,” she added. “There is also a social aspect to these groups, and I think we often see in Kaleidoscope and other groups that people tend to come more on a regular basis.”
For Young, one positive of the pandemic has been that people across society appear to be more willing to discuss mental health. She said that despite this promising trend, discussions are ultimately not enough.
“All of the self care and mental health general phrasing that is used needs to take that step further and acknowledge the ways that all of these systems that we live in actually directly impact our mental health,” she said.


_600_375_90_s_c1.jpg)