Counting Sheep? Don’t Neglect a Routine Sleep Schedule
Ryerson University Doctor to Speak at Concordia about the Dangers of Insomnia and Its Link to Depression
Pick two: sleep, study or socialize. According to this old adage, balancing all three is as much of an option as “magic wand” is in a game of “rock, paper, scissors.”
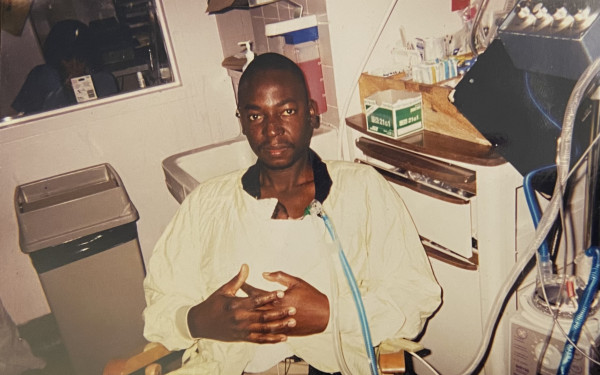
For Dr. Colleen Carney, too many students are following the trends of greater adulthood by neglecting a routine sleep schedule. Students are prioritizing their own academic success, altering their bodies’ internal clocks. According to Carney, this lack of routine is a main cause for chronic insomnia, which is a disorder closely linked to depression. She will address the issue at a talk at Concordia University on Tuesday night.
“That’s the big problem,” said Carney, who is the director of the Sleep and Depression Laboratory at Ryerson University in Toronto. “It’s that people don’t maintain a regular schedule, so many people are jetlagged without traveling.”
Carney noted that parental figures usually create strict schedules for children that mandate a consistent sleep time. She said humans don’t outgrow the need for this type of routine and dismisses the notion that sleep is a learnable skill.
“Sleeping is like falling in love,” said Carney, who is also an associate professor at Ryerson. “You can set the stage to make it more likely to happen—if you want to clean yourself [and] put yourself out there—[but] it’s something you can’t force to happen.
“The hallmark of an insomniac is somebody who believes that they have to do something to sleep.”
Many different diagnostic systems exist for chronic insomnia. Essentially, complaining about difficulty falling into or maintaining sleep for more than half the nights of the week in a three-month period is an indicator of the disorder. In addition, having daytime complaints of functioning, like mood or concentration problems and fatigue, are also telltale signs.
The National Institute of Health concluded in a State-of-the-Science Conference on Manifestations and Management of Chronic Insomnia in Adults that the condition is a major health problem affecting millions of individuals and their communities and families.
A term called “condition arousal” is also associated with chronic insomnia. It’s an unintentional learning that the body does so that when individuals get into bed, they suddenly feel wide-awake, according to Carney. Mentally linking a bed to a feeling of wakefulness occurs due to factors such as being “plugged into” mobile and laptop devices.
“Sleeping is like falling in love […] it’s something you can’t force to happen.”
The body has “beautiful” regulatory systems that compensate for occasional lack of qualitative and quantitative sleep, which works best within consistent bedding and waking times, Carney added. Too often, though, people—particularly students—are unable to utilize this bodily system. Late-night partying, early class times, substance abuse and even the stress of falling asleep contribute to chronic insomnia.
“Using alcohol or weed right before bed, these are things that, in the short term, may be helpful because you fall asleep faster,” Carney said about prevalent substance abuse in university. “But the quality of sleep under those substances [is] actually more negative [than] if you didn’t use it. It actually then starts disrupting sleep.”
A problem among psychiatric treatment providers is the belief that insomnia being a symptom of depression is not “meaningful,” Carney argued. It is believed that the sleep disorder is a symptom of depression that is relatively untreatable. Beginning with studies during her time at Duke University, Carney and other researchers found that over 50 per cent of insomniacs who recovered from depression relapsed.
Her team of researchers also discovered that a quarter of people with insomnia developed depression within a year’s time, while a little less than a quarter of the same sample developed an anxiety disorder. In addition, ten per cent of insomniacs turn to abuse of substances like alcohol. According to Carney, what is also commonly misunderstood is that many insomniacs are at increased risk of suicide.
“They think that it’s depression; it’s not,” she said. “People with insomnia are at risk of suicide and accidental overdoses because—think about a lot of celebrities who die this way—they’re very desperate to sleep.
“They start layering alcohol and hypnotic medication, and they just overdo it and die.”
To combat this sleep disorder, Carney and her team of graduate and undergraduate students from Sleep and Depression Lab are researching the merits of and training health practitioners in Cognitive Behavioral Therapy. CBT is a “multi-component” treatment that is recognized as effective by the NIH.
“If I had to sum it up, it essentially is that we study a person’s sleep patterns over the course of a few weeks and then we make an adjustment based on what’s going on with that person,” said Carney.
Adjustments include limiting the time patients spend in bed, enforcing regular, early wake up and bed times or curbing intake of coffee and the like. CBT is a brief treatment of one to four sessions that is just as effective as sleep medication, according to Carney.
“Unlike medication, it lasts for years and years,” she continued. “It’s a good investment for people.”
In no way, though, does Carney suggest that CBT is an exclusive alternative to traditional treatments for depression like medication. Instead she said that pairing CBT for insomnia with antidepressants could be most effective.
PERFORM Colloquium on Depression and Insomnia: Which Comes First and Why It Doesn’t Matter // Jan. 14, 4 to 5 p.m. // Room RF-120, Loyola Jesuit Hall and Conference Centre (7141 Sherbrooke St. W.) // Free



_600_375_90_s_c1.jpg)