STI stigma: Reinforcing the cycle
Navigating an STI diagnosis
On Nov. 13, Carl Nowack, grappling with a range of symptoms akin to a sexually transmitted infection (STI), made the decision to head to the hospital. The verdict was clear: he had gonorrhea.
Gonorrhea is an STI that can cause discomfort in the genital, rectal, and throat regions, typically treated within a few weeks with antibiotics.
The symptoms initially felt challenging, but reaching out to a healthcare provider brought relief. “Right after I got a shot of antibiotics and started my seven-day wait I was pretty relaxed,” he expressed.
The prevalence of sexually transmitted infections has been on the rise in Canada, with chlamydia, gonorrhea, and infectious syphilis rates experiencing significant increases between 2011 and 2019.
Gonorrhea has surged by 171 per cent, chlamydia by 26 per cent, and infectious syphilis by a staggering 389 per cent.
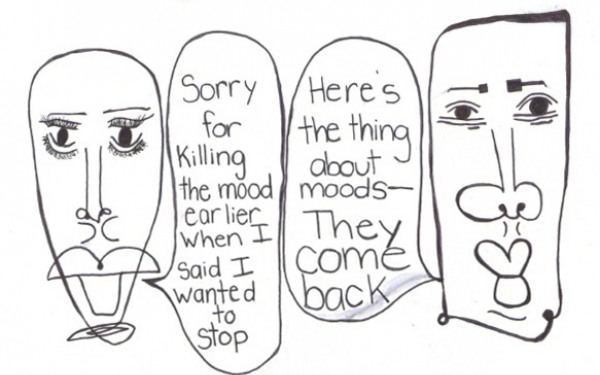
Nowack’s diagnosis prompted discussions in his surroundings about stigma and the mental challenges associated with such health issues. He reflected on the emotional impact and stated he didn’t even realize how getting an STI could change how he felt. “One thought I’ve had is just how this wouldn’t have happened if I wasn’t single, which re-opened some underlying feelings of loneliness,” he said.
According to Alex McKay, the executive director of the Sex Information and Education Council of Canada, “STI stigma discourages people from accessing testing for a bunch of reasons: they don't want to, they're embarrassed or they don't feel particularly comfortable interacting with healthcare providers because of that stigma.”
“There actually tends to be more stigma around those viral STIs than there is around bacterial STIs and the whole reason is that gonorrhea and chlamydia are very easily treatable,” added McKay. “So often when people are told they have human papillomaviruses (HPV), they panic, especially if they've been told it's incurable.”
According to WebMD, HPVs are often treatable, and a significant number of cases may exhibit no symptoms at all.
“We say that stigma kills because we have medications that allow human immunodeficiency virus (HIV) individuals to live as long as their peers who don’t have it,” said Olivier Renaud-Charest, a fourth-year medical student at McGill University, who is a part of the LGBTQIA2S+ community.
McKay explained that misconceptions frequently fuel the stigma surrounding sexually transmitted infections, as a dearth of education and a deficient understanding. A common misconception is that only individuals who engage in high levels of sexual activity or practice non-monogamy are susceptible to the impact of STIs.
“People who are serially monogamous and have one partner at a time, but end up over their life course with a number of sexual partners are all quite susceptible to STIs as well. So the kind of judgment that tends to come with STIs is completely counterfactual and unjustified,” McKay said.
Health Canada has recently approved new at-home HPV tests, offering a means to prevent cervical cancer.
Cervical cancer will affect 1 in 168 women in their lifetime, with 1 in 478 succumbing to it. The proactive use of appropriate testing has the potential to lower these numbers significantly.
This form of screening is becoming more common with the recent approval by the Food and Drug Agency for new at-home tests for chlamydia and gonorrhea.
“Overall, the concept of home testing for STIs is a good one because people, for a number of reasons including STI-related stigma, might be hesitant to visit a clinic or a doctor if they suspect they have an STI,” said Mckay.
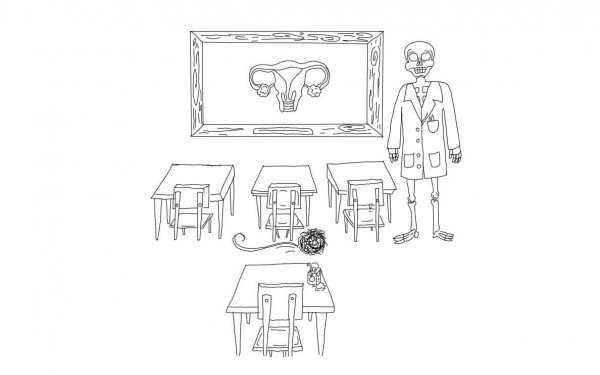
On campuses, other resources strive to combat stigma and advocate for comprehensive sex education.
The Sex and Self club strives to offer accessible resources within Concordia University, functioning as a chapter in a larger organization. One of its initiatives is the wellness pantry at Le Frigo Vert, providing various gender-affirming and safety items such as condoms, binders, menstruation products and more.
Although the club aims to be accessible to all, it tends to attract only a fraction of students.
“The people that really need to hear it, they might not be seeking it out,” said Muriel Smith, a film animation student and executive member of the Sex and Self club at Concordia University.
Upon receiving an STI diagnosis, a common response is an apprehension surrounding how others might react, coupled with internalized feelings of shame and guilt associated with the topic.
Smith shared a personal experience from a previous relationship where her ex-partner had dishonestly claimed to have transmitted an STI to her following their breakup, expressing, "I was not only scared for my health but also for my desirability.”
As for Nowack, he was grateful to have a positive response knowing it might not be the case for everyone who receives a diagnosis, saying, “it definitely was stressful to bring up, especially having to inform multiple partners. I would say I was lucky to have had really nice responses.”
Despite the federal government's efforts to raise awareness on the subject, there remains a lack of coherence in the education system. A recent study indicates that the Canadian sex education system is outdated and lacks a comprehensive understanding of the dimensions of sexual health.
“You can almost say it's normal to have been exposed to an STI at some point and that's not the general perception,” said McKay. “STIs do not discriminate in any way based on race, class, sexual orientation, gender identity, or any demographic factor, we are all susceptible to STIs and that's the information that we all need to know.”
This article originally appeared in Volume 44, Issue 7, published November 28, 2023.


_600_375_s_c1.png)